Cardiovascular disease (CVD) remains the leading cause of death in the United States.1 In the United States, disparities in CVD and associated risk factors exist among Black, Latino, and American Indian/Alaska Native individuals when compared with nonHispanic White individuals.1 Social determinants of health; the context in which people are born, live, learn, work, play, worship, age; and structural factors are regarded as the root causes of CVD disparities seen in these groups. Although there is a growing body of research identifying interventions that effectively address these longstanding racial/ethnic and socioeconomic disparities in CVD, many questions remain, and much of what we know is still not being used to change practice and policy. A growing body of knowledge also supports the notion that community-engaged research is a promising approach to promote cardiovascular health equity.
Community-engaged research is an exemplary model to mitigate this challenge because it transcends limitations associated with traditional scientific research and medical care models.2 By integrating a holistic approach, community-engaged research aims to understand individuals through a social, environmental, and cultural lens.2 Engaging communities throughout the design and implementation of studies allows for a greater understanding of their unique context or the social determinants that influence their health.2 Community-engaged research occurs along a continuum that can range from community outreach (eg, one-off, transactional events such as health fairs) and community consultation (eg, periodic requests for input or feedback) to community-based participatory research (CBPR), which involves authentic relationships with reciprocity, and ultimately, to community-driven research, which includes shared leadership with researchers, decision-making at the community level, and bidirectional trust.3 It is imperative that scientists and clinicians discontinue the common practice of taking time away from community members without giving back and rather strive to design studies that actively engage members through early inclusion, incorporation of ideas, and shared leadership, and that improve community health.4
CBPR, an illustrious form of community-engaged research, commits to the principles of co-learning by integrating community partners throughout the research study design, implementation, and dissemination of findings.4,5 Despite decades of evidence supporting the value of CBPR, uptake of these priniciples and practices across the scientific community remains limited. The CBPR framework of engaging stakeholders throughout the entire research process lends to sustainable solutions for the community and health policy changes that address health disparities.4 The foundational principles of CBPR are derived from the Northern Tradition practice of collaborative research centered on system changes and the Southern Tradition practice of emancipatory research that aims to expand research access and ownership.5 This collaborative research approach can encompass various research designs, including experimental, nonexperimental, case studies, longitudinal, ecological, and implementation science designs.5,6 CBPR leverages the unique strengths of academic and community partners through a framework that (1) promotes collaborative and equitable partnerships in all research phases and involves an empowering and power-sharing process, (2) recognizes community as a unit of identity, (3) builds on strengths and resources within the community, (4) facilitates co-learning and capacity building among all partners, (5) focuses on problems of relevance to the local community, (6) balances research and action for the mutual benefit of all partners, (7) disseminates findings and knowledge gained to the broader community, and (8) promotes a long-term process and commitment to sustainability.5 A key component of CBPR is that it enables academics an opportunity to reckon with medical mistrust and historic misgivings by empowering community members with equal decision-making power on research intended to benefit the community.6 Moreover, CBPR affords academics a clearer understanding of the community’s strengths, challenges, and opportunities, which lends way to creation of sustainable solutions.4
We have chosen to highlight a few studies that exemplify the principles of CBPR to promote cardiovascular health across the United States. Although not an exhaustive list, these studies clearly articulated how community engagement principles informed the design, implementation, and dissemination plans. The RICH LIFE Project, a pragmatic cluster randomized controlled trial in Maryland and Pennsylvania, compared the effectiveness of a health system only versus a health system in addition to a collaborative/stepped intervention to reduce disparities in hypertension.7 This project applied principles of CBPR, including the creating a diverse community advisory board that informed the entire research process; from formulating the research question, selecting study outcomes, and designing recruitment materials to implementation of the interventions, and suggesting dissemination approaches. The patient-centered and community-centered intervention also included community workers who provided social support and helped patients with linkages to community resources. This study is a unique exemplar of community-engaged research that sought to reduce racial, ethnic, and geographic disparities in hypertension and other cardiovascular disease risk factors using a pragmatic clinical trial design.
The Black Impact pilot study, based in a Midwestern city, has demonstrated that a community-based lifestyle change program improved Life’s Simple 7 scores among Black adult men at 12 and 24 weeks.7 First, a collaborative academic-community partnership between the African American Male Wellness Agency and a local academic institution was developed to design the program and refine the Diabetes Prevention Program curriculum. Refinements included the addition of mental health, physical activity, and nutrition information. A distinct feature of this study is that it was performed at recreation and park centers local to the targeted community.
The FAITH! Trial, a cluster-randomized controlled trial, tested the effectiveness of a community-informed mobile health intervention in improving the cardiovascular health of Black adults in Rochester and Minneapolis-St Paul, MN.8 This trial was built on over a decade of collaboration between an academic institution and Black churches to mutually prioritized the focus on promoting cardiovascular health. A unique feature of this CBPR academic community partnership was the co-design of a mobile health application for Black adults and the establishment of a steering committee which comprised of academic-community partners and other stakeholders.
The THRIVE Study is a unique CBPR study that implemented a healthy retail intervention to improve the intake of healthy fruits and vegetables and food purchasing behaviors in convenience stores that serve Native American communities in the Chickasaw and Choctaw Nations of Oklahoma.9 Community-engaged research to promote the cardiovascular health of Native American people is uncommon. The study was led by a steering committee that included academics, Tribal citizens, employees, and leaders from government, commerce, and health sectors in both nations. The steering committee met monthly to establish financial and research agreements between the academic institutions and the two Nations. This study was conducted in direct response to a finding that food insecurity was associated with chronic disease in Native populations. Thus, CBPR was used to tailor the intervention to the unique context of Native people, which are affected by economic and structural forces that impede access to healthy foods.
A hallmark of these exemplar studies is authentic, ongoing partnerships between academic institutions and communities to promote cardiovascular health in populations that bear a disproportionate burden of CVD. A deep commitment to best practices in community engagement is required to advance the cardiovascular health of historically excluded and socially disadvantaged populations that are at higher risk of adverse CVD outcomes, as an approach to advancing health equity. These principles include power sharing and the formation of an equitable partnership in all aspects of the research process, from the conceptualization to the dissemination of the findings. It is also critical that opportunities are created for capacity building of community members, including hiring from the community that is participating in the research and building on existing resources in the community. We must rethink the traditional model of one-off projects that do not have plans for sustainability or translation of findings into local policies that improve the health of communities. Adherence to the core tenets of community engagement also requires a substantial time commitment to understanding the community’s context, engaging key community stakeholders, and a careful balance of research priorities and community needs (Figure).
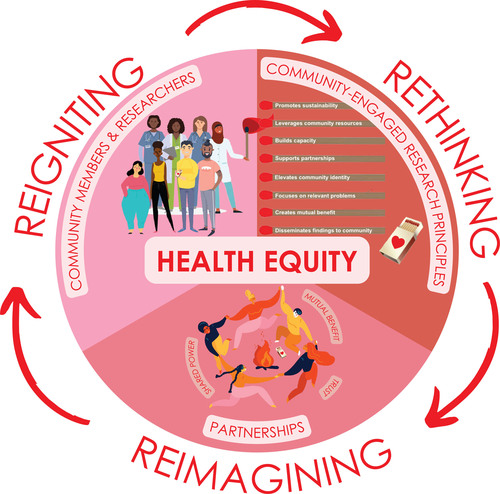
Figure. Rethinking, reimagining, and reigniting community-engaged research to promote health equity.
Although community-engaged research is a promising approach to reducing the burden of CVD, there are several gaps that must be addressed. These include limited studies among Latino populations, refugee and immigrant populations, Native American people, gender and sexual minority groups, and persons with disabilities. Furthermore, few studies have reported on the evaluation of the academic community-partnership functioning, which limits our understanding of how to enhance these partnerships to improve health outcomes. This gap may be attributed to the lack of consensus on the ideal evaluation and partnership building approaches. Furthermore, there is a critical need to further explore interventions and approaches that can successfully recruit, retain, and activate groups that have experienced social marginalization in community-engaged research studies.
Community engaged research holds great promise for advancing cardiovascular health and health equity through transformed systems that support people in achieving their best health. In February 2022, the National Academy of Medicine’s Organizing Committee for Assessing Meaningful Community Engagement in Health and Health Care Programs and Policies developed a new conceptual model that provides several lessons for all who seek meaningful community engagement to advance health equity.10 We must reimagine partnerships among researchers, practitioners, health systems, and communities as being inclusive and diverse, and as reflecting sustained relationships with shared power, mutual benefit, and trust (Figure). Then, we must use these partnerships to expand knowledge, improve health and healthcare programs and policies, and create thriving communities. It has been said that imagination is where we go, not only to escape painful realities, but also to create new and better realities. When we use our reimagined partnerships to design cardiovascular health and healthcare programs and policies of the future, we create new images of our communities that reignite community members and researchers, regardless of scientific discipline and stage of research along the translational science spectrum, with motivation to act (Figure). This renewed motivation is what our partnerships can use to directly address or adapt to contextual factors such as social, political, economic, and environmental influences on health, and the drivers of change in these factors, realizing the vision of opportunities for all to attain optimal health.

